Chronic, low-grade inflammation links to cardiometabolic conditions such as type 2 diabetes and coronary heart disease. Diet can influence inflammatory markers, including C-reactive protein (CRP), which clinicians use to assess systemic inflammation. A daily pattern rich in fibre, unsaturated fats, and polyphenols can support a healthier inflammatory response.
This guide reviews practical anti-inflammatory foods to include each day, with clear examples and portion-friendly ideas. It focuses on ingredients that fit common meals and snacks, helping you build consistency without relying on supplements or restrictive rules.
Key takeaways
- Prioritise oily fish like salmon or sardines for omega-3 anti-inflammatory fats.
- Use extra virgin olive oil as a main fat, replacing butter and refined oils.
- Eat a wide range of colourful fruit and vegetables to increase polyphenol intake.
- Add nuts, seeds, and pulses for fibre that supports a healthier gut microbiome.
- Choose wholegrains over refined carbohydrates to reduce blood sugar spikes.
- Include spices such as turmeric and ginger regularly to boost antioxidant compounds.
What inflammation is and how diet influences inflammatory markers
In 2021, an estimated 17.9 million deaths were linked to cardiovascular disease worldwide, and chronic inflammation contributes to atherosclerosis and plaque instability (WHO: cardiovascular diseases). Inflammation is the immune system’s chemical response to injury or infection, but persistent, low-grade inflammation can keep inflammatory markers elevated even without an acute threat. Clinicians often track this activity using blood tests such as high-sensitivity C-reactive protein (hs-CRP); values above 3 mg/L indicate higher cardiovascular risk compared with levels below 1 mg/L (CDC: C-reactive protein).
Diet influences these markers through fatty acid balance, fibre intake, and the density of polyphenols (plant bioactives). For example, the Dietary Guidelines for Americans recommend keeping saturated fat below 10% of daily energy intake, because higher intakes tend to raise LDL cholesterol and can amplify inflammatory signalling (USDA: Dietary Guidelines). By contrast, diets that emphasise unsaturated fats, whole grains, and vegetables often correlate with lower hs-CRP and improved insulin sensitivity, two measurable drivers of inflammatory load. Even modest shifts matter: a 5% energy swap from saturated to polyunsaturated fats is associated with meaningful reductions in cardiometabolic risk in large cohort analyses.
Extra-virgin olive oil and nuts: key sources of anti-inflammatory fats
At lunch, swapping a buttered baguette for a salad dressed with extra-virgin olive oil and a small handful of walnuts changes the fat profile of the meal within minutes. A 15 ml tablespoon of extra-virgin olive oil provides about 14 g of fat, most of it monounsaturated oleic acid, while a 28 g serving of walnuts adds roughly 2.5 g of plant omega-3 (ALA) alongside polyphenols.
This matters because the type of dietary fat influences inflammatory signalling. Extra-virgin olive oil contains phenolic compounds such as oleocanthal, which shows ibuprofen-like activity in laboratory models, and higher-polyphenol oils have reduced oxidised LDL in controlled trials. Large cohort data also support the pattern: higher olive oil intake associated with lower cardiovascular and total mortality in long-term follow-up (Harvard T.H. Chan School of Public Health: olive oil).
For broader daily use, treat extra-virgin olive oil and unsalted nuts as default fats rather than occasional “healthy extras”. Aim for 1–2 tablespoons of extra-virgin olive oil across meals and 20–30 g of nuts most days, adjusting for energy needs. Choose oils labelled “extra-virgin” and store them away from heat and light to protect polyphenols and limit oxidation.
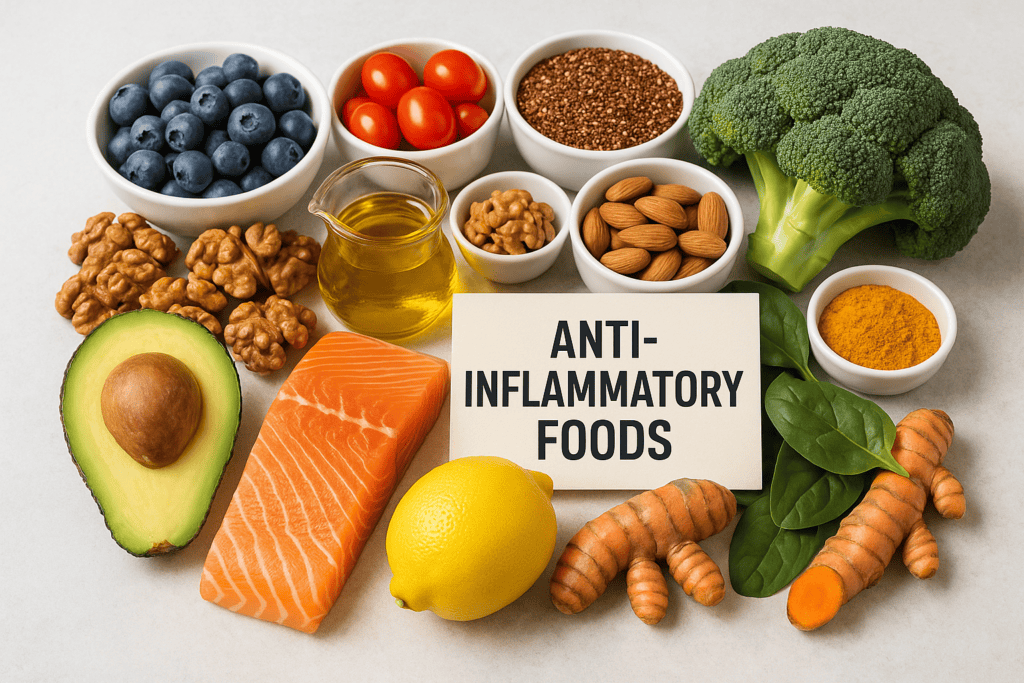
Anti-inflammatory foods
Oily fish and seafood: omega-3 foods to eat weekly
Oily fish provides long-chain omega-3 fats (EPA and DHA), while most other proteins supply little or none. Salmon, sardines, mackerel and trout deliver EPA/DHA directly; chicken, eggs and most plant proteins rely on conversion from ALA, which remains limited in adults.
| Option | Main omega-3 type | Typical EPA+DHA per serving | Practical note |
|---|---|---|---|
| Salmon (cooked, 100 g) | EPA + DHA | Often ~1.5–2.5 g | Reliable weekly staple; choose grilled or baked. |
| Sardines (canned, ~90–100 g) | EPA + DHA | Often ~1.0–1.8 g | Low-cost option; check salt content on the label. |
| Prawns or white fish (100 g) | Small amounts of EPA + DHA | Often <0.5 g | Lean protein; pair with an oily fish meal to meet targets. |
Key differences matter because EPA and DHA influence inflammatory signalling and triglycerides more directly than ALA. For most adults, a practical target is two fish portions per week, including at least one oily portion, aligned with NHS guidance. A standard portion equals about 140 g cooked fish.
Practical implications include choosing gentle cooking methods and managing contaminants. The FDA and EPA advise prioritising lower-mercury seafood; pregnant people and children need stricter limits. If fish intake stays low, discuss omega-3 supplements with a clinician, especially when taking anticoagulants.
Vegetables, fruits, and legumes: high-polyphenol and high-fibre staples
Most UK adults fall short of fibre targets, which matters because low fibre intake links with higher C-reactive protein (CRP), a common inflammatory marker. The Scientific Advisory Committee on Nutrition (SACN) recommends 30 g of fibre per day, yet average intake sits closer to 20 g. Plant variety also matters: the ZOE PREDICT programme popularised 30 different plant foods per week, which correlates with a more diverse gut microbiome.
Vegetables, fruits, and legumes help because they supply polyphenols (bioactive compounds that influence inflammatory signalling) and fermentable fibre that gut bacteria convert into short-chain fatty acids. Those fatty acids support the gut barrier and can reduce inflammatory activity. A 150 g portion of cooked lentils provides roughly 12 g fibre, while 80 g of raspberries adds about 5 g, making the daily target achievable without supplements.
Start with one legume serving per day: add 120–150 g cooked chickpeas to lunch, or swap half the mince in a chilli for 200 g canned beans (drained). Aim for five portions of vegetables and fruit daily, using the NHS 5 A Day guidance (80 g per portion). Use “colour stacking” at dinner: include at least three colours (for example, spinach, red peppers, and purple cabbage) to widen polyphenol intake.
After 2–4 weeks, many people notice easier bowel regularity and steadier appetite, while clinicians often see improved fibre-related markers such as lower LDL cholesterol. Increase legumes by 50–75 g every 3–4 days and prioritise well-cooked beans to reduce bloating.
Herbs, spices, and beverages: turmeric, ginger, green tea, and coffee
A meta-analysis of randomised trials reported that curcumin supplementation reduced C-reactive protein (CRP) by about 0.8 mg/L versus control, indicating a measurable shift in systemic inflammation (see PubMed for indexed trial reviews). In parallel, a large umbrella review found that habitual coffee intake associated with lower all-cause mortality, with the lowest risk typically observed at around 3–4 cups per day. These figures matter because herbs, spices, tea, and coffee deliver concentrated polyphenols that can influence oxidative stress and inflammatory signalling without adding large amounts of energy.
Turmeric and ginger stand out because small culinary doses can meaningfully raise polyphenol exposure. A practical target is 1–2 teaspoons (about 2–6 g) of turmeric powder across meals, paired with black pepper to improve curcumin absorption; piperine can increase curcumin bioavailability by up to 2,000% in pharmacokinetic studies. Ginger works well at 1–2 g per day (roughly ½–1 teaspoon ground, or a 2–3 cm fresh piece) in soups, stir-fries, or yoghurt-based dressings.
Green tea supplies catechins, especially EGCG, which researchers link to lower oxidative stress markers. One brewed cup (250 ml) typically provides about 50–100 mg of EGCG, depending on leaf quality and steep time. Two to three cups per day often fits well with hydration goals while keeping caffeine moderate for most adults.
Coffee contributes chlorogenic acids and other polyphenols, but preparation and timing affect tolerance. For many people, 2–4 cups per day aligns with the range most consistently associated with benefit in population studies, while remaining within the European Food Safety Authority (EFSA) guidance of up to 400 mg caffeine per day for healthy adults. Choose filtered coffee when possible, since paper filters reduce diterpenes that can raise LDL cholesterol.
- Easy daily pattern: turmeric in eggs or lentils, ginger in porridge or stir-fries, 2 cups of green tea, and 1–2 filtered coffees.
- When to be cautious: anticoagulant use, gallbladder disease, pregnancy, or reflux can change suitability; confirm with a clinician if unsure.
Practical daily meal structure: portions, frequency, and food swaps to reduce inflammation
At 07:30, a common breakfast is a large bowl of sweetened cereal with fruit yoghurt and a latte. That combination can exceed 35–45 g of free sugars in one sitting, while providing under 5 g of fibre, which leaves little room for the 30 g daily fibre target set by SACN. By 11:00, hunger often returns, and the next choice tends to be a refined snack rather than a balanced meal.
A practical anti-inflammatory structure starts by anchoring each eating occasion to three measurable elements: 20–30 g of protein, at least 8–10 g of fibre, and a source of unsaturated fat. For breakfast, swapping cereal and yoghurt for 170–200 g plain Greek yoghurt plus 30 g oats, 150 g berries, and 15 ml extra-virgin olive oil or 20–30 g nuts typically lifts fibre into the 10–12 g range while cutting added sugars to near zero. That shift supports steadier glucose exposure, which matters because higher post-meal glucose links with higher inflammatory signalling in metabolic studies.
Apply the same template at lunch and dinner: fill half the plate with vegetables or legumes, keep starchy carbohydrates to a fist-sized portion, and replace butter, cream, and processed meats with olive oil, fish, beans, or yoghurt-based sauces. Over a week, this pattern makes it easier to reach 25–30 g fibre per day and to keep oily fish at 1–2 servings, without complex tracking.
Frequently Asked Questions
Which anti-inflammatory foods have the strongest evidence for reducing C-reactive protein (CRP) levels?
Foods with the strongest evidence for lowering C-reactive protein (CRP) include:
- Extra-virgin olive oil (about 20–50 g/day in Mediterranean-style diets)
- Fatty fish providing 1–2 g/day EPA+DHA (for example, salmon, sardines)
- Tree nuts (about 30 g/day, especially walnuts and almonds)
- High-fibre foods adding 25–38 g/day fibre (oats, beans, berries)
How many servings of oily fish per week support an anti-inflammatory diet, and what portion size should you aim for?
Aim for 2 servings of oily fish per week to support an anti-inflammatory diet. Target a portion size of about 140 g cooked fish per serving (or roughly 100 g when tinned). This intake typically provides around 250–500 mg per day of EPA and DHA omega-3 fats, which help regulate inflammation.
Which spices and herbs provide measurable anti-inflammatory effects, and what daily amounts are commonly used in studies?
Studies most often use turmeric (curcumin) 500–1,000 mg/day, ginger 1–2 g/day, garlic 600–1,200 mg/day (or 1–2 cloves), cinnamon 1–3 g/day, and rosemary extract 200–500 mg/day. Common culinary herbs such as oregano and thyme also show effects, typically at 1–2 teaspoons/day dried.
How can you build an anti-inflammatory breakfast using wholegrains, fruit, and protein without excess added sugar?
Build breakfast around minimally processed wholegrains (porridge oats, rye, barley) and aim for 30–40 g fibre per day. Add 1–2 portions of fruit (berries, apple) for polyphenols, then include 20–30 g protein (Greek yoghurt, eggs, tofu, nuts). Avoid flavoured yoghurts and sweetened cereals; use cinnamon or vanilla instead.
Which common foods and ingredients can increase inflammation, and what practical swaps reduce exposure to them?
Foods linked with higher inflammation include sugary drinks, refined grains (white bread), processed meats, deep-fried foods, and products high in trans fats and omega-6 seed oils. Practical swaps:
- Water or unsweetened tea instead of sugary drinks
- Wholegrains instead of refined grains
- Beans, fish, or poultry instead of processed meats
- Olive oil, nuts, and seeds instead of fried snacks
